Why is patient bathing important?
Patient bathing is an essential nursing activity. For immobile patients, a bed bath is the only solution to maintain hygiene and stay fresh. The main goal of patient bathing is to enhance the quality of life and well-being of the patient. With patient bathing, sweat, oil and microbes on the skin are also removed and body odour can be decreased.1
In addition, patient bathing plays an important role in preventing hospital-acquired infections and preserving skin integrity, and it presents a good opportunity to assess the skin integrity of a patient. For decades, the traditional patient bathing procedure has been used, but opinions are starting to change.
What is the traditional patient bathing procedure?
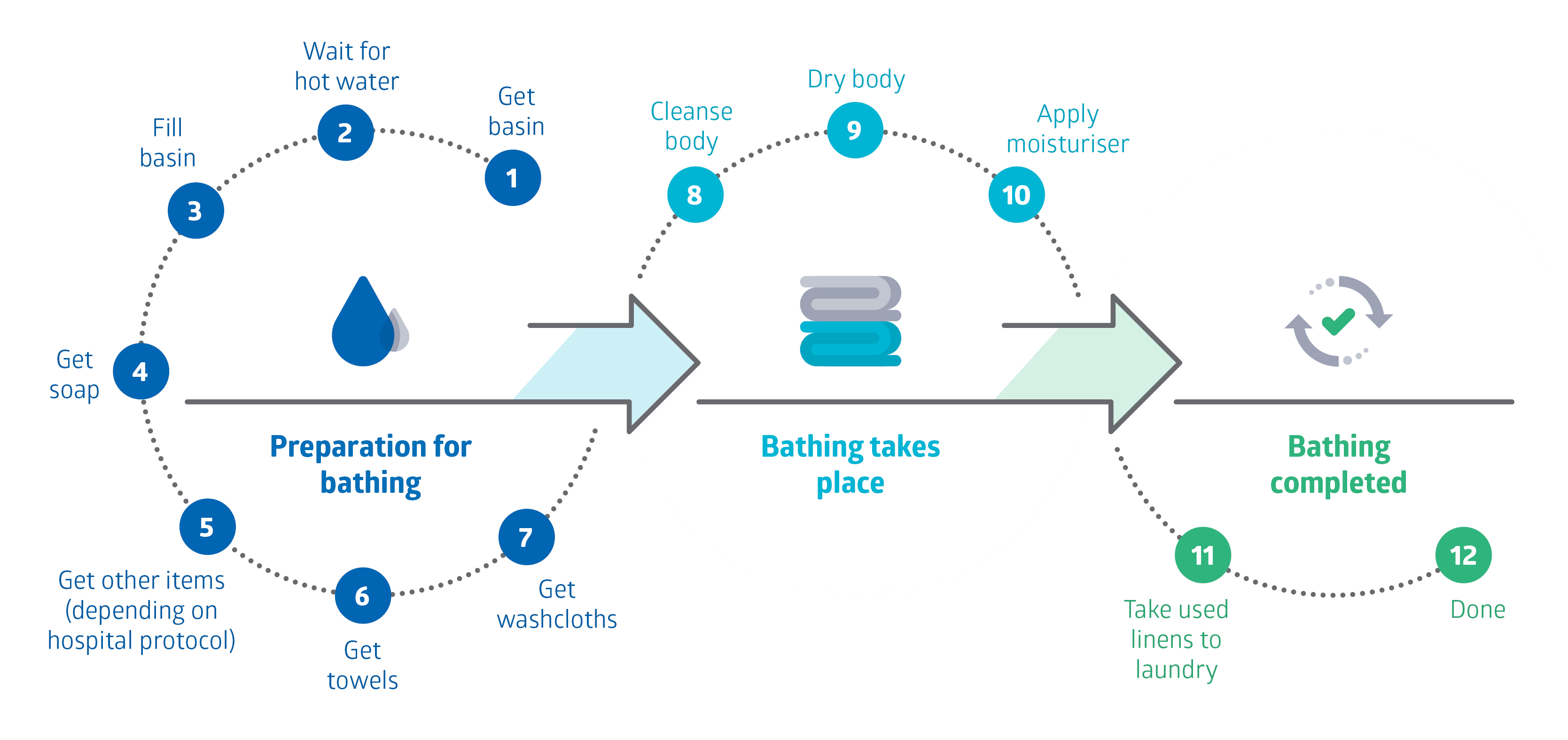
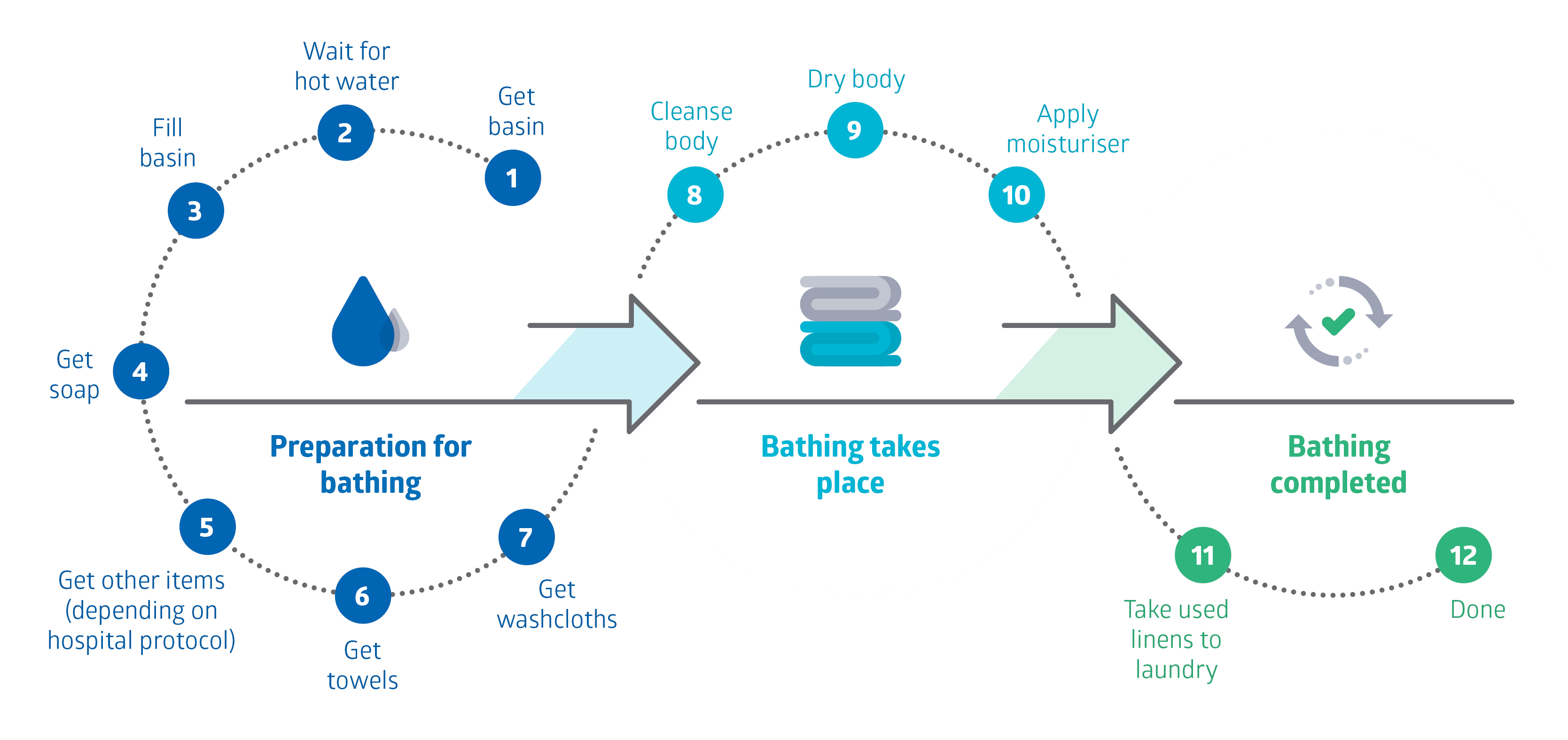
The traditional method consists of various elements like basins, soaps, towels and moisturisers, as you can see below. Often, the protocol in hospitals is to start with the cleaner parts of the body and end with the buttocks. During the procedure, cleaning, drying and applying the moisturiser to the body requires going over the patient’s body three times. In the stressful ICU environment, where nurse-to-patient ratios are generally low, this means that nurses need to dedicate a good amount of time to a single patient just for bathing.
Adverse effects of traditional patient bathing
In the last 30 years, healthcare professionals and researchers have started to question the effectiveness of the traditional basin bath method. There have been numerous studies examining the effectiveness of the traditional method in terms of patient comfort, nurse comfort and infections. All of this research concludes that the traditional bathing procedure comes with some adverse effects:
- Patients might feel uncomfortable, insecure or undignified during the bathing procedure.2
- Traditional basin bathing has the risk of cross-contamination. Studies have shown that basins are frequently contaminated with microbes, and some studies even found that bacteria grew in up to 98% of the basins.3,4 If the basin disinfection procedure is not thorough enough, the risk of cross-contamination between body parts or between different patients exists.
- Using water, soap and towel drying can cause dry skin, and dry skin can impair skin integrity.1
- The water supply for bathing might contain pathogens that can cause hospital-acquired infections.5
- When repositioning bedridden patients for bathing, there is always a risk of injury for the nurses.
- Usually more than one nurse is needed to complete the bathing procedure, which takes around 30 to 40 minutes, taking their time away from more urgent tasks.
- With traditional bathing, the risk of spills is present, which can cause slipping/falling, damage to the electronic devices around the patient bed, and spills on the bed—making it necessary to change linens.
Patient bathing solutions
All of these adverse effects, and the general questioning of the effectiveness of the traditional patient bathing procedure have led to the development of alternative methods. In recent years, disposable skin-cleansing cloths, especially disposable washcloths, have become more commonly used.
Disposable cloth packs usually include 8 impregnated cloths for 8 different areas of the body (enough for one ‘bath’). After each cloth is used, it is disposed of. Using disposable washcloths offers lots of advantages due to the elimination of basins and limited contact of washcloths with different body parts. It also provides a more practical bathing process, for both healthcare staff and patients.
We will talk in detail about the new patient bathing method in our next blog post. In the meantime, if you want to check out Medline’s patient bathing products, you can have a look at our catalogue.


Zeynep Ergeneci
Product Manager ReadyCare, Personal Care, Advanced Wound Care and Repositioning & Offloading, Medline Europe
Zeynep, originally from Turkey, came to the Netherlands in 2020 to complete her Master of Science in Economics. She graduated in 2021 and completed an internship in sales analysis. After that, she joined Medline Europe and is currently managing Medline’s urology and ReadyCare portfolios. Zeynep has a passion for travelling, exploring new cultures and really enjoys nature. Learn more on Linkedin.
References:
1. Veje, P., & Larsen, P. (2014). The effectiveness of bed bathing practices on skin integrity and hospital-acquired infections among adult patients: a systematic review protocol. JBI Database of Systematic Reviews and Implementation Reports, 12(2), 71–81. https://doi.org/10.11124/jbisrir-2014-1422
2. Lopes JL, Nogueira-Martins LA, de Barros ALBL. Bed and shower baths: comparing the perceptions of patients with acute myocardial infarction. J Clin Nurs. 2012;22:733–40. doi:10.1111/j.1365-2702.2012.04320.x.
3. Johnson D, Lineweaver L, Maze LM. Patients bath basins as potential sources of infection: A multicenter sampling study. American Journal of Critical Care. 2009; 18(1): 31-38.
4. Greaves A. We`ll just freshen you up, dear. Nursing Times.1985; 5: 3-8.
5. Anaissie EJ, Penzak SR, Dignani MC. The hospital water supply as a source of nosocomial infections. Arch Intern Med. 2002;162(13):1483–92. doi:10.1001/archinte.162.13.1483.



