During the 2020 – 2021 period, the number of people visiting the accident and emergency (A&E) department at the East Kent University Hospital Trust (EKHUFT)—one of the largest in the south-east of the UK—increased by up to 25%. However, the more alarming development had to do with a noted surge in cases of falls, particularly those resulting in severe harm.
The associated risks were, therefore, clear for everyone to see:
- A&Es were busier than they have ever been.
- The quality of health across the population of patients seeking help in A&Es was declining.
- Those seeking help had longer-than-usual waiting times in A&E departments.
- There was no clear way for staff to indicate which patients they have assessed as having a high risk of falling.
Falls with harm are not only devastating to patients and families. But there are also considerable financial implications for healthcare providers. For example, the estimated cost of a single fractured neck of femur or hip (#NoF) is £26,000.1 In 2020 alone, EKHUFT recorded five such #NoF cases in just one A&E—representing a bill of £130,000 (excluding possible litigation costs).
How then can we prevent falls in the healthcare/A&E environment? Through my experience with a recent trial on visual cueing, we will answer this important question using a simple four-step approach that we developed as part of our FallStop programme.
FallStop 4 step approach
Step 1: Ensure you have the support of everyone in the department and senior management
Having supported A&E staff with patient falls incidents, I was aware of how upsetting this was to them, particularly their inability to identify effectively, at a glance, whether a patient was at risk of falling.
While each nurse customarily has patients assigned to him/her, issues would arise at the handover point. This would happen very quickly and there was little to tell in terms of which patients were most at risk of falling—until it was too late.
At this point, having worked within A&E departments and acute medical assessment units, I knew they needed something eye-catching and unique to help raise their awareness and keep them vigilant.
Step 2: Integrate visual cues into the care protocol to help staff manage patients at high risk of falling
What visual cueing materials did we apply to the above-mentioned situation? It is a lot simpler than you might be imagining. It was a falls kit containing a small yellow fleece blanket and a pair of yellow double-tread falls prevention slipper socks.
Why choose/use this particular kit?
The kit in question includes items that are designed to stay with the patient throughout hospitalisation, regardless of location in the healthcare environment. These items can also go home with the patient.
Additionally, the yellow kit reminds all staff that extra precautions need to be taken with particular patients, and that they should act decisively if they see such a patient mobilising unassisted or attempting to get off the trolley. This yellow-themed solution also helps ward staff during patient transfers, as each patient has already been identified as a falls risk, triggering a full fall risk assessment, in line with Trust policy/guidelines.


Step 3: Make a case for the financial impact of not taking action
There is nothing more frustrating than knowing there is a simple solution that works and falling short of implementing it because others, whose support you need, just see additional costs. The initial mindset may be ‘That sounds expensive!’
There is a way forward. You must show, in a powerful way, the extent of the financial burden the organisation would have to carry, should it choose to ignore the problem or only address symptoms. As we have learned, the total cost of care for a hip fracture was £26,0001 and there have been not one, but five neck of femur fractures in the A&E.
The challenge is to prove the effectiveness and value of visual cueing as an appropriate intervention. For that, we developed a single site evaluation with clear outcomes. The key to this initiative was to have the support from the A&E matron, sisters and senior management. This meant that, as the results of the evaluation emerged, everyone involved could see the benefit and share in the success of the initiative. Essentially, it started to develop its own momentum. We can change the initial mindset to a more informed and practical one: ‘That solution could help us protect our patients and cut long-term costs at the same time!’
Step 4: Education before, during and after
The A&E-based evaluation was well controlled and allowed us to clearly show the effectiveness and value of the yellow kits. However, it only worked because:
- Everyone within the department knows to which patients they are to issue specialised falls yellow products
- Other staff working with A&E (clinical and non-clinical) understand the need for extra vigilance around those patients wearing them.
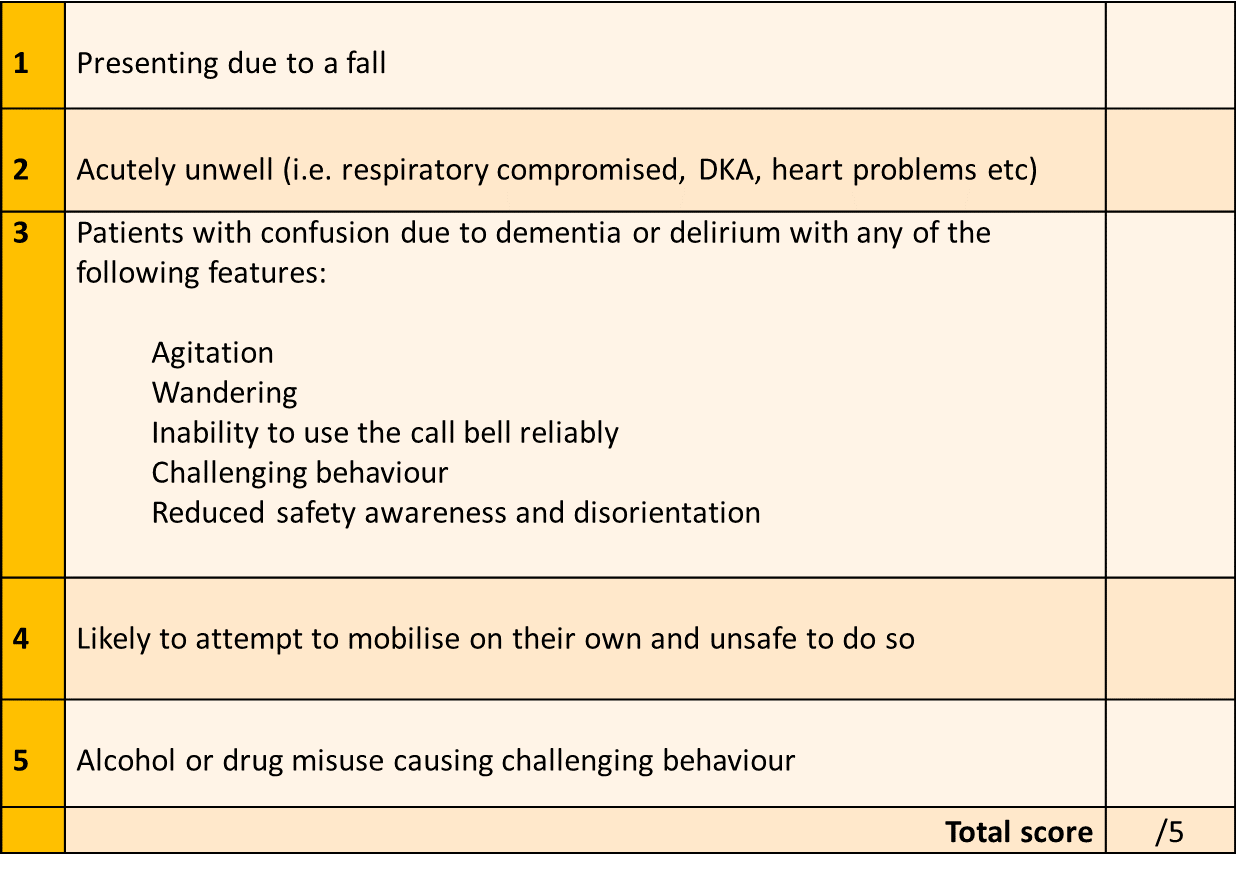
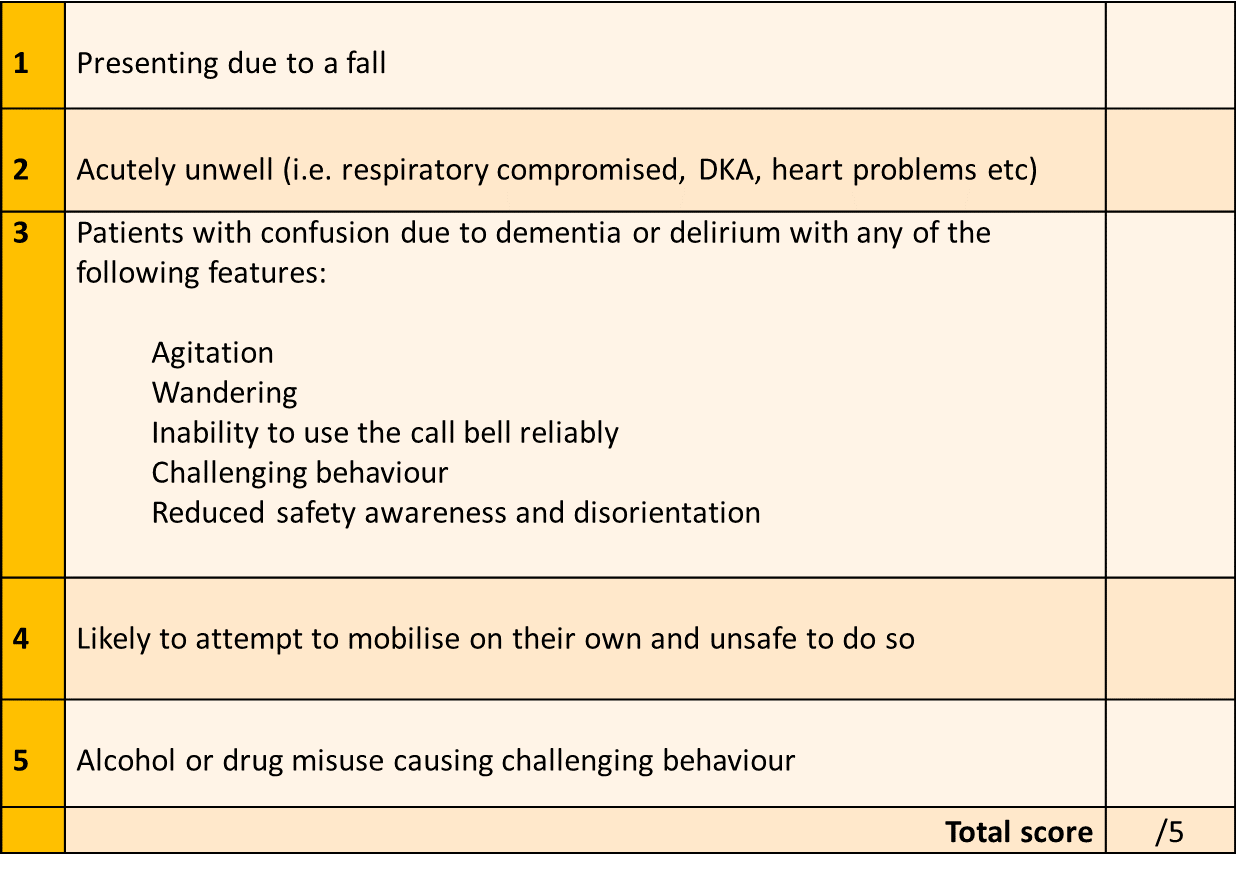
To help you, here is a list of five criteria for ensuring you select the right patients. If a patient fulfils two or more, they should be issued with a yellow kit.
Think Yellow!
Staff in and around the A&E must all be aware of the yellow kits and understand what they mean.
Medline, supplier of the kits, also provides many educational materials like posters for staff notice boards, storerooms and public spaces.
To complement that, we involved our communications team to help promote it through the staff newsletter and on the intranet. We even got our Chief Executive on board and she promoted the project through her podcast. However, the most important part of the evaluation, by far, was spending time with the staff in A&E, particularly in the early stages to ensure they fully understood when to use the kits and what they meant.
During the evaluation, I was able to review and recommend several harm prevention strategies for newly admitted patients. We followed their hospitalisation journey and none of those patients fell. Medline’s yellow kit empowered A&E staff to think and work differently, as well as made them feel unique to be part of this highly effective initiative.
So, was it worth it? In short, yes. 100%!
The trial ran for six weeks, and over this period, we lowered the number of falls by 50%. In fact, the only patients who fell were those who did not have a yellow kit. The story was also the same for patients admitted to wards. Not one fell in the first 24 hours, which is the period when most falls would usually happen on wards.


Jayne Flood
Falls Prevention Practitioner, East Kent Hospitals NHS Foundation Trust
Jayne has worked as a Falls Prevention Practitioner for the last five years. Prior to this, she worked on the emergency floor as an Associate Practitioner with clinical skills galore. Patient safety has always been a passion of hers, especially preventing patient falls. She recently completed an online falls prevention course and has worked tirelessly to provide a falls service for her Trust. Jayne continuously works to develop the necessary services to ensure quality improvements are implemented, ensuring patients are as safe as they can be.
Going back to the beginning, Jayne started her working career 31 years ago as an Auxiliary Nurse. She then went on to complete her NVQ level 2 and 3 and her NVQ assessor course, which allowed her to assess and train her colleagues, including student nurses and HCAs. After that, Jayne went on to complete a foundation degree.
References:
1. NHS Digital10/21
2. National Institute for Clinical Excellence, Quality standard for hip fracture, August 2016








